The acronym BED has nothing to do with sleep. It stands for Binge Eating Disorder, a condition that was found in the old DSM-IV only in its appendix. Since the 1994 publication of that edition of the DSM, nearly 1,000 papers about BED have been published. When changes for the revision of the manual were being discussed, some critics objected to its promotion to the main body of the book because, Sharon Kirkey wrote:
They wonder how reliably doctors who are not experts in eating disorders can distinguish between someone who binges for psychiatric reasons and someone who merely overeats.
The doubts were in part protective, because a lot of folks could be incorrectly branded with a mental disorder diagnosis or given psychiatric drugs when they didn’t need them. In the litigious United States, discontinuing an obese person’s employment under these circumstances could be interpreted as discrimination against the mentally ill.
The chair of the DSM-5 work group for eating disorders, whose job it was to decide what to include in that section of the manual and what to leave out, was psychiatry professor Dr. Timothy Walsh. Not all obese people have BED, and not all people with BED are necessarily obese. Compared to other varieties of obese people, those with BED have “substantially higher frequency of mood and anxiety problems,” Dr. Walsh explained to the reporter. The unhappiness is the difference.
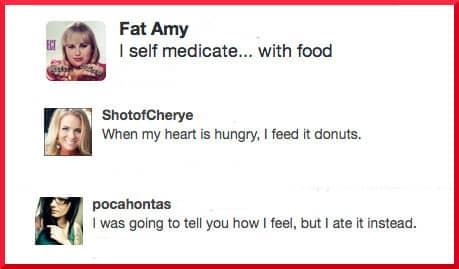
“It is not what is eating you… but what you are eating”
Dr. Vera Tarman further noted that BED is not the same as food addiction, though the populations of the two disorders overlap. One difference she sees is that people suffer from BED in response to “what is eating them” – in other words, emotional trauma that they attempt to self-medicate by extreme consumption. What they need instead is healing for the PTSD, anxiety, or depression that drives the behavior. Tarman says,
Treatments include cognitive therapy, mindfulness and medications. They are taught how to eat all foods moderately, in the hopes that they were join “normal society” once their psychological conditions have been addressed, even resolved.
For the food addict, the problem is “what they are eating” – refined starches, sugar, or whatever problem food of which a single taste can trigger a cascade of unwise ingestion. She sees the cravings for these foods not as resulting from distressed emotional states, but from addictive qualities inherent in the foods themselves.
Certainly emotions can trigger a person to want to eat, but the control is lost truly when the food has ignited the reward pathway in the limbic brain….While psychological issues are important to sustain long term recovery, the essential first treatment for the food addict is to stop the drug that is creating the loop of addictive eating….Treatment includes abstinence from the triggering foods, peer support to encourage ongoing vigilance, and often a spiritual dimension needs to be tapped into to maintain long term recovery.
Food addiction was never recognized by the older DSM editions (nor is it acknowledged by the current DSM-5), which Dr. Tarman calls “a poor reflection of our clinical reality.” As with BED, there are pros and cons to official recognition of food addiction as a bona fide medical condition, and opinion is divided.
The lack of official recognition of food addiction means that insurance providers won’t pay for treatment, which Tarman describes as a “dire consequence.” Once a person is morbidly obese, bariatric surgery may be funded, but not treatment for the addiction that caused the weight to accumulate.
On the other hand, being labeled as an addict can have serious consequences for the patient. Taking a broader view, a fear also exists of the “overarching ambition” of some factions to medicalize everything that strays just a bit over the line drawn around normal behavior, for the purpose of selling another million pills and undeservedly enriching the pharmaceutical industry.
Source: “Binge eating to become bona fide entry in disorder bible,” Canada.com, 04/29/10
Source: “Binge Eating Disorder in the DSM 5: Good News or No News for the Food Addict?”
Addictionsunplugged.com, 01/30/13
Image by Fat Amy, ShotofCherye, pocahontas

 FAQs and Media Requests:
FAQs and Media Requests: 











