Inside UCLA’s Fit for Health Program

As we’ve written time and time again, childhood obesity is a complex condition shaped by far more than diet and exercise alone. At UCLA Health’s Fit for Health Program, clinicians are embracing a comprehensive model that treats obesity as a medical, emotional and social condition — one that requires coordinated, compassionate care. Let’s take a quick look at what works in the current environment and what the challenges are.
Founded nearly 15 years ago by Dr. Wendelin Slusser, a UCLA Health physician specializing in clinical care, medical training and obesity research, the program has long focused on improving outcomes for children and adolescents. Since 2024, however, the clinic has expanded its reach and scope under new leadership.
Dr. Vibha Singhal, who took over the program last year, said she broadened its approach by integrating new therapies, obesity medications and bariatric surgeries related to weight loss. Beyond treatment, the clinic also serves as a learning environment, with undergraduates, medical students, residents, and fellows contributing to patient care.
Research is a central pillar of the program’s mission, Dr. Singhal said, noting:
I have my own lab where we have studies primarily around obesity and obesity treatments… Addressing food insecurity, how we can build that into our program, evaluating for potential eating disorders, evaluating the newer medications and the risks of infertility effects on the next generation.
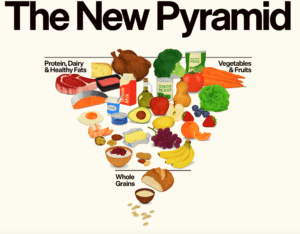
Addressing food insecurity and eating disorders
For many families, access to healthy food remains a barrier to care. The program currently uses a small food bank grant to help clinicians address food insecurity among patients, Dr. Singhal said.
Eating disorders are another common challenge. Many patients struggle with binge eating and related conditions, according to Dr. Singhal. To meet these needs, the clinic relies on a multidisciplinary care team that includes psychologists, nutritionists and social workers who collaborate closely.
Dr. Natacha Emerson, the program’s psychologist, said:
We are sort of a one-stop shop… Unlike going to a doctor’s visit, where they just refer you to a psychologist or a dietitian, all three of those providers are actively working together to focus on shared goals to make sure that we are helping patients the way that they want to be helped.
Rapid growth brings new challenges
The demand for this integrated model of care has surged. Since October 2024, the clinic’s patient volume has doubled, Dr. Singhal said. To keep up, the program added two new physicians and expanded availability for nutritionists and psychologists.
Still, growth has brought strain. Dr. Singhal said:
We doubled the volume, but we didn’t double all our resources… It adds a lot of work on the team… It’s getting hard to keep up.
Insurance coverage remains a significant hurdle as well. Many obesity treatments are not covered, and Dr. Singhal said she anticipates further medication cuts at both the state and federal levels starting in January.
Serving vulnerable families
The clinic often serves families who are underinsured or undocumented, which can make accessing care difficult. Dr. Emerson noted that fear and uncertainty around immigration status can discourage families from seeking medical help. She said:
In the last year, we have had a lot of our patients who want to be healthier and have healthier bodies, but some of our families also have parents that are undocumented, and that has made seeking health care scary in this certain climate.
Telehealth has helped bridge that gap. According to Dr. Singhal, the clinic’s no-show rate has dropped as families increasingly return for care, including through video visits. Dr. Emerson offered:
Thankfully, we’re able to keep patients via video visit, which is sometimes a good way to make people feel more secure, especially when there are transportation and other barriers to getting to the clinic.
Integrating mental and physical health
A defining feature of the Fit for Health Program is its commitment to addressing mental health alongside physical health. Dr. Emerson said part of her role is identifying mental illnesses that may be influencing a child’s weight, allowing the team to intervene early and appropriately.
Dr. Singhal also shared a long-term vision for the clinic: creating a structured program specifically for patients with developmental disabilities, including autism, Down syndrome and genetic disorders.
Meanwhile, the program’s social worker, Bobby Verdugo, leads a mindfulness initiative that helps families navigate complex social and behavioral challenges. He said:
We tailor the (mindfulness) curriculum to the family… Some families may want to work a lot on portions, some want to work more on what they’re eating too fast and others on physical activity. We really adjust it to the family and I think that’s pretty unique — the ability to provide this intervention, to customize it to the family and then to continue to work with families in this kind of holistic, multidisciplinary way.
Redefining success beyond the scale
For many young patients, emotional well-being is just as important as physical health. Dr. Emerson said children often arrive with negative body image and pressure to be thinner rather than healthier — an expectation the clinic works to gently reshape.
At UCLA’s Fit for Health Program, progress is measured not just in pounds lost, but in confidence gained, barriers reduced and families supported, which we believe is an approach that reflects the true complexity of childhood obesity.
Speaking of UCLA…
Dr. Pretlow, the creator of BrainWeighve, a weight loss app for overweight and obese children, is conducting a BrainWeighve clinical trial at UCLA. The trial has expanded to include 10 subjects currently taking GLP-1 medications. This addition aims to help researchers understand how lifestyle and behavioral tools enhance medication or possibly even reduce the need for medication over time.
The program is designed for obese teens and uses a self-directed, physician-supervised approach to tackle overeating one “problem food” at a time. By helping participants rechannel emotional urges into healthier coping mechanisms, BrainWeighve aims to support sustainable weight loss — and reduce dependence on willpower alone.
Your responses and feedback are welcome!
Source: “UCLA Fit for Health Program adopts holistic approach to childhood obesity,” Daily Bruin, 1/14/25
Source: “Fit for Health Program,” UCLA.org, undated
Image by Los Muertos Crew/Pexels








 FAQs and Media Requests:
FAQs and Media Requests: 











