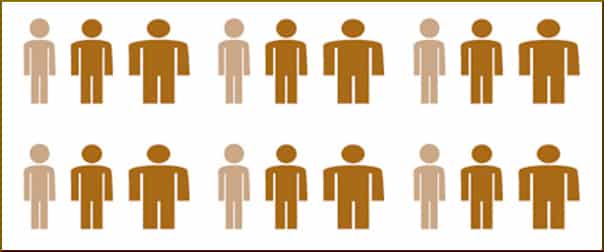
By now, it is well-known that minority children and youth are much more likely to be overweight or obese, but here is a disturbing fact about weight-loss surgery in the United States. Such a procedure is twice as likely to be performed on a white teen.
Various experts have suggested reasons for this disparity. Primary care physicians may not be up to speed on the seriousness of obesity as a disease. There might be a poor understanding of both the benefits and risks. It could be due to inadequate insurance and ineligibility through governmental medical care programs.
In the case of Spanish-speaking patients, it has even been suggested that the language barrier might be a factor. Or it may be because outcomes have been shown to be much less satisfactory.
Boston Medical Center researchers report that “African Americans and Hispanic Americans who have undergone Roux-en-Y gastric bypass (RYGB) are at greater risk to regain weight as compared to Caucasians.” This was clarified by corresponding author Nawfal W. Istfan, M.D., Ph.D.:
Racial or ethnic differences in food choices and eating behaviors have long been linked to obesity and cardiovascular disease. However, it is unclear whether there are racial differences in RYGB-mediated changes in appetite hormonal signals, mental health and eating behaviors.
The Kaiser Family Foundation learned that, of 52 million Hispanics under the age of 65, 21 percent were uninsured, as compared to 13 percent of blacks and only 9 percent of whites. A nationwide survey of nearly 80,000 patients revealed that “obese Hispanics were less likely than persons of the other two races to undergo weight-loss surgery.”
Dr. John Magana Morton of Stanford University opined to a reporter that the disparity is not caused by discrimination, because “Hispanics tend to be less insured than Caucasian or African American patients — as well as preference for patients to go to nonacademic centers,” he said.
Questions of responsibility
But, as we have seen, poverty leads to lots of bad consequences including obesity and its co-morbidities, and it just so happens that many people of color are found in the lower socio-economic strata. Quite likely, the very fact of being uninsured can frequently be traced back to discrimination. Looking down from a more secure place in the economic hierarchy, it is easy to mistake necessity for preference. Maybe poor people go to “nonacademic centers” because they lack choice.
For long-term recovery, a patient needs a stable environment and a robust support network. In general, a kid from a family with money is more likely to have those things. For people who live in constant economic struggle, the environment is more likely to be chaotic, and not particularly amenable to the long-term maintenance of weight loss, or sobriety, or anything, really. A family in the midst of being evicted, for example, is not optimally positioned to help anyone.
The bigger picture
Dr. Sarah Barlow of the Baylor College of Medicine takes bariatric surgery very seriously, comparing it in terms of risk to an organ transplant. She points out that severely obese children need access to the lifestyle programs that should come first, and although some insurers will cover the surgery itself, they balk at the kind of intensive counseling that is really needed, both pre- and post-operatively. She warns,
We need to ensure that availability and coverage are fair… It would be a disservice to children if primary care providers could easily refer to bariatric surgery but had no place to refer for comprehensive, multicomponent behavior-based treatment.
Indeed, another recent study concluded that “efforts to reduce racial variation in the use of weight loss surgery should focus on eliminating socioeconomic barriers and educating patients before they are referred to surgery.”
Your responses and feedback are welcome!
Source: “Obese minority children less likely to have weight-loss surgery,” Reuters.com, 09/15/17
Source: “Race plays role in regaining weight after gastric bypass surgery,” MedicalXpress.com, 11/15/18
Source: “Hispanics trail blacks, whites in bariatric surgery rates,” MDEdge.com, 11/22/17
Source: “Teens Gain Big Benefits From Bariatric Surgery,” NJBariatricSurgeons.com, 01/01/16
Source: “Patient race and the likelihood of undergoing bariatric surgery among patients seeking surgery,” September 2016
Image by Pat Hartman

 FAQs and Media Requests:
FAQs and Media Requests: 











