Globesity — A Young Doctor in South Africa
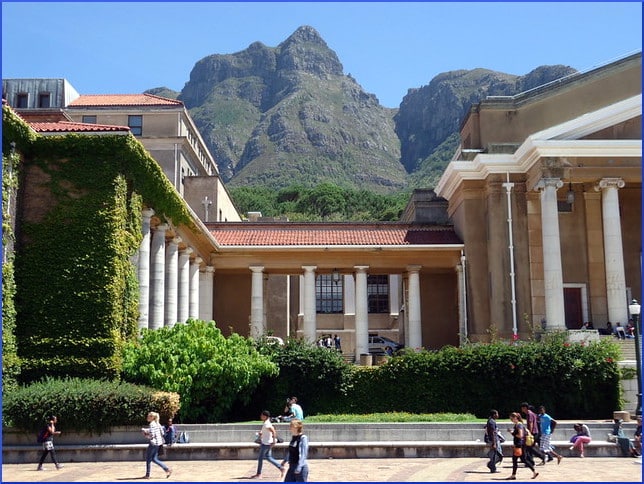
A dispatch from the University of Cape Town described part of last year’s summer program, a two-day course led by Dr. David Hume, who was awarded his Ph.D. at the school where he continues to pursue additional credentials to become a physician-scientist. One lecture was titled “The Obese Brain: The Neuroscience Behind Weight Gain.”
The other was called “Optimising Obese Interventions”, which fits in with our recent examinations of connections that have been sought or tried in the areas of smoking cessation and ending alcohol addiction. Hope is always high that success in one problem is transferable to another.
Dr. Hume’s subject matter was divided into five categories: birth, bacteria, the brain, the food industry, and eating behaviors. (He did not succumb to temptation to go for total alliteration by calling the last two simply Behavior, and Big Food.)
Carla Bernardo reports for the University of Cape Town News that the neuroscientist…
[…] looked at the three systems that are implicated in weight gain and the obesity phenomenon. He also explored the endocrine system’s relationship with insulin and ketones, the nervous system’s response to input from the gut, and eating behaviors.
Dr. Hume talked about the importance of vaginal birth in populating a newborn’s microbiome, and described the functions performed for us by our friendly interior bugs. When a neuroscientist speaks, naturally the brain will come into it. Scientists have suspected for a while now that the gut bacteria and the brain have a communications system.
Bernardo describes two examples the lecturer gave of this hotline, one having to do with serotonin and the other with the immune system:
Serotonin is the hormone that promotes an overall a state of well-being, deficiencies of which have been implicated in mental disorders such as depression. Over 90 percent of serotonin is produced in the gut.
The second instance of crosstalk is that gut bacteria link up with important immune cells in our gastrointestinal tracts. They cause a series of changes that sends a signal to the brain to act early to protect itself against any harm.
The big news about the microbiome is that we have more power over it than we have over a lot of other things. Apparently, our dietary choices can influence the activities of friendly bacteria to an inordinate degree. Dr. Hume compares this very personal territory to a garden where each person can decide what to cultivate, and if we make the right choices, the microbiome will confer upon us many benefits.
A major problem he sees is the cheapness and easy availability of sugar. But many substances contribute to the encouragement of overconsumption. Dr. Hume says,
What has happened is the people in the food industry have become masters at manipulating the food that we consume. Food has been altered to the point that it packs an extra pleasure punch which has now been scientifically termed as the “bliss point” in food.
It’s really frightening to consider that food which has the potential to alter our guts, our organs and our brains is being tampered with to the extent that itʼs altering our actual brain tissue… The good news is that a bad gut is reversible.”
Your responses and feedback are welcome!
Source: “The science of the obese brain,” uct.ac.za, 01/15/19
Photo credit: Ian Barbour on Visualhunt/CC BY-SA









 FAQs and Media Requests:
FAQs and Media Requests: 











